Seizures & Epilepsy
General Information
What is it?
Abnormal neuronal excitatory activity
Epilepsy: two or more unprovoked seizures within 24 hours or 60% recurrence rate after the first
Risk Factors: trauma to the affected bone, young age ([extreme] sports), old age (osteoporosis, brittle bones)
Evaluation:
- Symptoms
- Trigger
- Aura (present only in focal seizures): sense of deja vu (disconnect with temporal lobe), nausea, automatisms (rapid blinking, lip smacking/chewing)
- Ictal event: seizure
- Post-ictal phase (in focal seizures with impairment, full generalized seizures, or focal to bilateral generalized): confusion, lethargy, amnesia, Todd’s paralysis (unilateral weakness)
- Physical exam
- Obtain history (mechanism of injury, timing/progression, prior injury)
- Inspection, palpation, evaluate range of motion (ROM)
- Imaging: x-ray (first line, include joint), CT (complex fractures), MRI (stress)
- Lab biomarkers:
- Bio formation markers (alkaline phosphatase, calcium, phosphate)
- CBC: increased WBC recruitment
- CRP/ESR: elevated due to inflammation
Classification(see below)
- Focal seizures
- Generalized seizures
Pathophysiology:
Greater electrical activity can be attributed to decrease in inhibitory pathway (GABA) or increase in stimulatory (glutamate)
Glutamate pathways
- Increased production
- Increased AMPA/NMDA receptor activity
GABA pathways
- Dysfunctional GABA-A receptors (which facilitates hyperpolerization), diminishing GABA’s inhibitory effects
Physiological Blurb: AMPA vs NMDA Receptors
AMPA
- Ionotropic: Na+, K+
- Phasic
- Activation: voltage-independent glutamate binding
NMDA
- Ionotropic: Na+, K+, Ca2+
- Has Mg2+ block at RMP (thus not open)
- Tonic
- Activation: glutamate-induced depolarization (removing Mg2+ block)
Etiology
VITAMIN D N E mnemonic for seizure causes:
Vascular, Infectious, Traumatic, Autoimmune, Metabolic, Idiopathic, Neoplastic, Drugs, Extra
Vascular: ischemic/hypoxic brain injuries, hemorrhage
Infections (CNS)
Traumatic brain injuries: epidural/subdural hematoma
Autoimmune: lupus, neoplasias
Metabolic: Na+, Ca2+, Mg2+ imbalances, increased T3/T4, ammonia
Idiopathic: see Epileptic syndromes
Neoplastic: gliobastomamultiforme, meningioma, metastasized malignancies
Drugs (Otis Campbel): opioids, tricyclic antidepressants, isoniazid, salicyclic toxicity, cocaine, amphetamines, metronidazole, penicillin, benzo withdrawal, ethanol, lithium
Extra/other: ecclampsia, genetic/family history
Classification
Focal seizures
Consciousness
Focal aware (simple partial): retain consciousness
Focal impaired awareness (complex partial): lose consciousness
Motor
Focal clonic: rhythmic jerking
Focal myoclonic: brief, shocking jerk
Focal clonic (Jacksonian March): jerking spreads along motor homunculus, starting distally and moving proximally (ex. jerking originates in hand but moves up to full arm)
- EEG findings: contralateral motor spikes
Non-motor
Focal sensory (originating in parietal/occipital/temporal lobes): pain, parasthesias, hallucinations, ringing, abnormal, intense smells
Focal autonomic (originating in insula): SNS symptoms (increased HR, TA, HT), urinary incontinence, salivation
Focal cognitive/emotional: deja vu, hypersexual, depersonalization
Generalized seizures
Motor
Grand Mal (tonic-clonic) classic convulsive: starts tonic (stiffening) then clonic (jerking) with extreme contractions
- EEG findings: polyspike-and-waves, high amplitude spikes
- Contractions: lungs (involuntary scream), eyes (extreme upgaze), mouth (pooling of oral secretions), mastication (jaw clenching, tongue biting), sphincters (incontinence)
Focal secondarily generalized (focal to bilateral tonic-clonic): focal hemisphere origins then progress to tonic-clonic
Tonic: see above
Clonic: see above
Myoclonic*: asynchronous rapid jerking
- EEG findings: 10-16 Hz polyspike wave bursts
Atonic: no movement, drop attacks
Non-motor
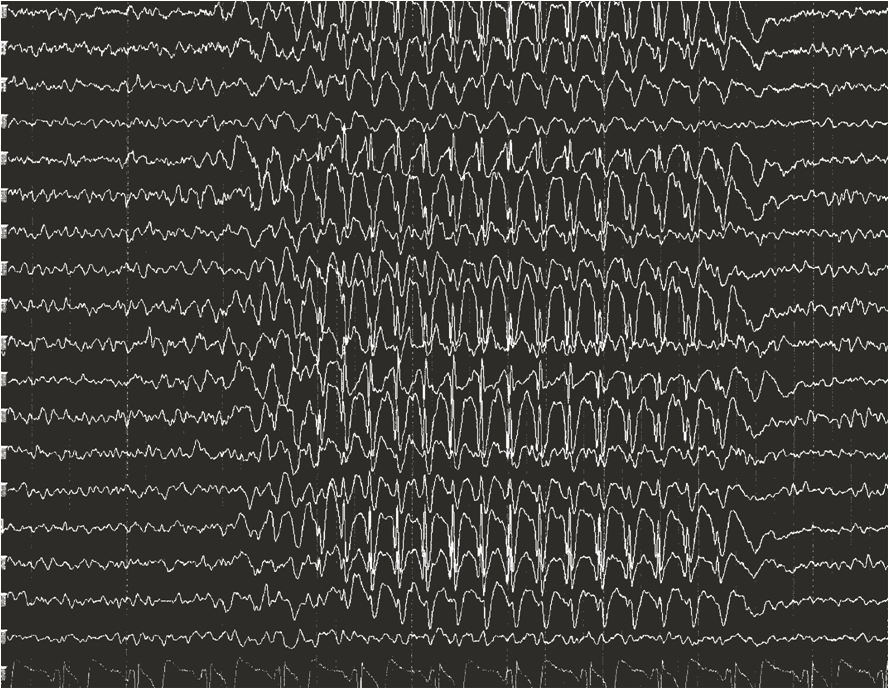
Petit mal (absence): “star-gazing” (dazed, unresponsive), no post-ictal phase
- EEG findings: 3 Hz spike-wave (Figure 1)
*Note: all generalized seizures, except myoclonic, present with complete/brief impairment
Epilepsy
Definition: two or more unprovoked seizures within 24hrs OR 60% recurrence rate after the first
Epileptic syndromes
- West syndrome: severe, brief jerky spasms in infants (linked to developmental encephalopathy)
- Lennox-Gastaut syndrome: severe, childhood onset of multiple seizure forms (tonic, atonic)
- Juvenile myoclonic epilepsy: jerking movements in waking, generalized seizures
- Dravet syndrome: severe infantile epilepsy (often fever-triggered)
Status epilepticus: extremely urgent, >5 min continuous seizures OR recurrent seizures without return to normal electrical activity
Treatment
To counter glutamate’s excitatory effects
Anti-epileptics
- Na+ channel blockers (very problematic to let phosphenytoin cuddle): valproic acid, phosphenytoin, topiramate, lamotrigine, fosphenytoin, carbamazepine
- Prevent positive influx of ions, reducing rate of depolarization
- Ca2+ channel blockers: gabapentin, ethosuximide (especially for absence)
- Prevent Sv2a-mediated vesicular exocytosis of glutamate
- Sv2a blockers: levatiracetam
- AMPA/NMDA antagonists: ketamine
To increase GABA’s inhibitory effects
- GABA-A agonists (mimic GABA activity): benzodiabepines, propofol, phenobarbital
- GABA reuptake inhibitors: tiagabine
- GABA-transaminase inhibitors (which normally inactivates GABA): vigabatrin, valproate


Leave a comment