Fractures
General Information
What is it?
Disruption in typical bone morphology, structure, and continuity
Risk Factors: trauma to the affected bone, young age ([extreme] sports), old age (osteoporosis, brittle bones)
Evaluation:
- Symptoms
- Pain (immediate, worsened by movement/weight-bearing)
- Edema from the inflammatory response
- Ecchymosis
- Systemic symptoms: fever, tachycardia (infection secondary to open fractures)
- Physical exam
- Obtain history (mechanism of injury, timing/progression, prior injury)
- Inspection, palpation, evaluate range of motion (ROM)
- Imaging: x-ray (first line, include joint), CT (complex fractures), MRI (stress)
- Lab biomarkers:
- Bio formation markers (alkaline phosphatase, calcium, phosphate)
- CBC: increased WBC recruitment
- CRP/ESR: elevated due to inflammation
Classification (see below)
Pathophysiology:
- Applied force (Fa) exceeds natural deformation/stretch capacity of bones
- Fracture healing pathophysiology (see below)
Classification
Categorization (Simple)
Position
Nondisplaced (ends of the bone retain normal position) vs Displaced (ends of the bone do not retain normal position—misaligned)
Completion
Complete (bone completely broken) vs Incomplete (only certain areas of the bone are affected)
Penetration
Open/Compound (bone passes through epidermis, is visible) vs Closed/Simple (is retained below visible tissue)
Direction
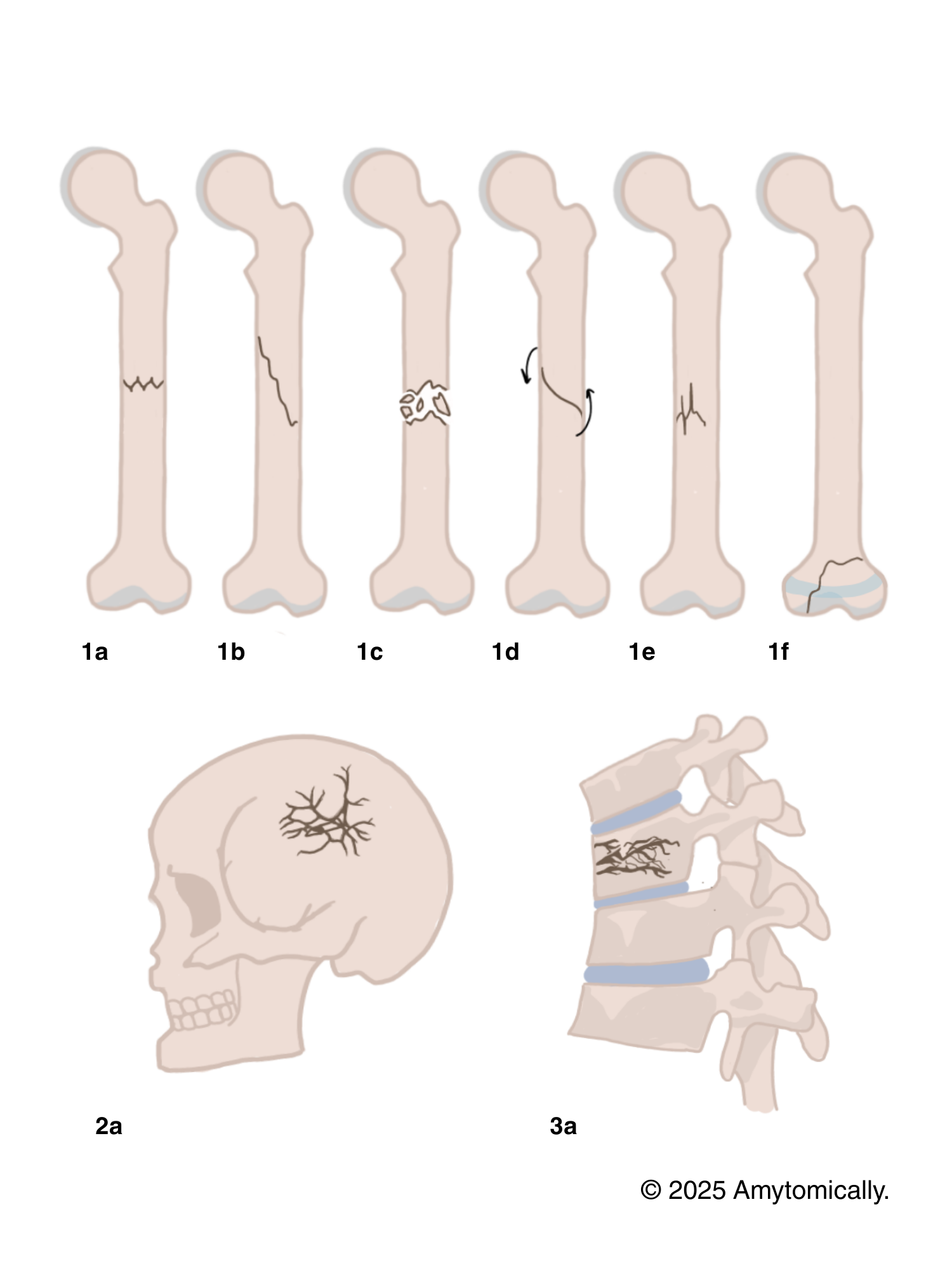
Transverse (horizontal; Figure 1-1a) vs Oblique (diagonal; Figure 2-2a)
Categorization (Specific)
Comminuted (Figure 1-1c): 3 or more bone fragments produced (high impact trauma or falls)
Compression (3a): crushing forces/bone collapse in the vertebra (most commonly due to osteoporosis)
Spiral (1d): caused by twisting/corkscrew forces, primarily in long bones
Epiphyseal (1f): occur in the epiphyseal/growth plate, where matrix and cartilaginous growth are still occurring in youth
- May cause long-term limb deformities, since occur in growing epiphyses
- Are graded by the Salter-Harris classification system (see below)
Depressed (2a): cranial bones pressed and dented inward
Greenstick (1e): incomplete fracture where bone breaks on one end, bending on the other (especially in children’s softer bones)
..& many more!
Salter-Harris Classification
Classifies physeal fractures and injuries of children only to determine severity
Salter I (slipped)
Fracture line extends through or within the epiphyseal plate; typically due to longitudinal forces
Ex. mild sports injury fall
Salter II (above)
Fracture extends through epiphysis and metaphysis; most common
Thurston-Holland fragment (corner sign): a small corner of the metaphysis is still visible
Ex. falling onto outstretched hand (FOOSH) injuries
Salter III (lower)*
Intra-articular fracture from physis into epiphysis; may form two epiphyseal segments
Ex. ankle injuries with sudden stops/turns (skiing)
Salter IV (through/transverse)*
Fracture passes through epiphysis, physis, metaphysis; may affect articular cartilage
Ex. motor vehicle collisions, high-impact sports
Salter V (rammed)*
Crush or compression fraction of the epiphyseal plate
Ex. falling from extreme heights
*Carry the greatest risk for long-term or chronic bone/joint deformities, growth retardation.
Physiological Blurb: Fracture Healing
1. Hematoma formation (1-7 days)
Formation of a large fracture hematoma (clot) in the affected area disrupts circulation, killing local osteocytes
Platelets release PDGF, TGF-b
Inflammatory cells, markers (IL-1, IL-6, TNF-a, VEGF) recruit osteoprogenitors and mesenchymal stem cells
2. Soft callus formation (1-3 weeks)
Migration of fibroblasts (produce collagen) and chondroblasts (restore cartilaginous matrix) from surrounding periosteum and endosteum
Provide initial stabilization and support, splinting broken bone
3. Hard callus formation (3-8 weeks)
Osteoblasts secrete matrix (endochondral ossification) around fibrocartilaginous soft callus, gradually replacing it with a harder, bony callus
4. Remodeling (months-years)
Bony callus remodeled into lamellar bone: excess material exterior to the diaphysis and in the medulla is removed
Osteoclasts resorb woven bone, osteoblasts secrete lamellar bone
Treatment
- Reduction: realignment of broken bone ends
- Closed (external) reduction: coax bone ends into position
- Open (internal) reduction: bone ends secured surgically with screws and plates
- Immobilization: cast or traction
- Medication:
- Pain control (acute): acetaminophen, opioids (if severe)
- Infection risks (open fractures): antibiotics (cephalosporin, penicillin)
- Bone healing: calcium/vitD, biphosphonates (for long-term osteoporosis-induced compression fractures)


Leave a comment