Aortic Dissection
General Information
What is it?

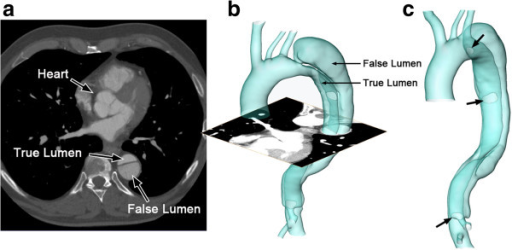
A relatively uncommon, high mortality disorder characterized by a tear through the aortic tunica intima and into the tunica media (layers of the aortic wall), forming an intimal flap and a false lumen
Stanford’s Classification:
- Type A: involving the ascending aorta; requiring surgical intervention
- Type B: distal to left subclavian artery down to descending aorta (only involves descending aorta); medial therapy or surgical intervention
Risk Factors (causes delineated in more detail below): hypertension (HT), genetic connective tissue disorders, atherosclerosis, family history, surgery, trauma
Evaluation:
- Primary symptomatology includes “tearing” and/or sharp pain
- If the tear occurs in the aortic arch, the pain might present as radiating into the neck/jaw or anterior chest
- If the tear occurs in the descending aorta, AD might present as interscapular/shoulder pain
- Secondary or nonhallmark characteristics: neurological deficits, ischemia, symptoms of AD-induced complications
- EKG to rule out differentials
- Imaging
- *CT angiogram: first line gold standard; can identify intimal flap, false lumen
- Chest x-ray: widened mediastinum (>8cm), pleural effusion
- Transesophageal echocardiography (TEE): for patients who are hemodynamically unstable (CTA unavailable); can identify true and false lumen, potential thrombi
- Laboratory pearls
- D-dimer test: may rule out AD if nonelevated
Pathophysiology:
- Tear leads to the creation of the true and false lumen
- Blood can flow through the lumen, inducing:
- (1) Rupture of the vessel wall (may present as hypotension) and high risk of mortality following
- (2) Hematoma formation which occludes the attached branching blood vessels inducing malperfusion syndromes (see right)
Malperfusion Syndromes
Location of AD →
Coronary vessels
Effects
Myocardial infarction, cardiac tamponade, regurgitation murmurs
Kidneys/renal system
Acute kidney injury due to low urine output resulting from ischemia
Artery of Adam Kiewicz
Anterior spinal arterial syndrome (spinal cord ischemia, paraplegia)
Other arteries: GI, lower extremity
Mesenteric ischemia (if compromised mesenteric arteries), acute limb ischemia (if iliac)
Causes & Etiology
Hypertension (HT)
The most common cause, especially in Type B patients who are older
Pathophysiology: (1) Blood pressure alone can cause the tear; (2) high BP can induce atherosclerosis causing a tear secondary to a weaker intima and necrosis due to low perfusion
Connective tissue (CT) disorders
Marfan syndrome:
- Presents as long extremities and above average height, hypermobile joints, accompanying cardiovascular issues (abnormal fibrillin synthesis contributes to decreased vessel elasticity and increased risk of AD)
Bicuspid aortic valve (instead of normal three cusps: see Valves)
Coarctation of the aorta (CoA):
- Narrowing of aorta typically near the subclavian: increased pressure proximal to narrowing leads to a similar high BP situation responsible for AD
Vasculitis
Inflammation of vessels due to syphillis, cocaine
- Syphilllis induces inflammation of vaso vasorum, increasing tear susceptibility
Iatrogenic origin
Heart surgery may lead to aortic injury or tears, particularly aortic instrumentation (e.g., PCI catherization, coronary artery bypass, valve replacement)
Pregnancy
Treatment
Surgical intervention (Type A or B)
Open heart surgery:
- Excise tear site and remove false lumen entry points
- Polyester graft to reconstruct aorta
- Valve reconstitution if aortic valve affected
Type B AD cases requiring surgery (i.e., causing malperfusion syndromes, aortic rupture) typically involve endovascular stent placement
Non-surgical (Type B)
For blood pressure: beta blockers, ARBs, ace inhibitors, calcium channel blockers
Lifestyle changes: smoking habits, diet (especially if hypercholesteremia)
Hypotensive therapies: vasopressors, give fluids (i.e. IV)


Leave a comment