Alopecia
General Information
What is it?

Loss or absence of hair characterized by varying etiologies, with the most common being the nonscarring or reversible alopecias (androgenetic “pattern hair loss”, alopecia areata, and telogen effluvium)
Risk Factors: family history of hair loss, older age, significant hormonal changes (e.g. childbirth, menopause), autoimmune disorders (e.g. thyroid), genetic predisposition
Evaluation:
- Hair pull test: grabbing 40-60 strands of hair → if ≥ 6 strands of hair are pulled, could indicate further cause of concern for telogen effluvium or alopecia areata
- Terminal to Vellus hair ratio: ≤3:1 qualifies for nonscarring alopecias
- Visualization of baldness or lack of hair
- Low ferratin or Vitamin D3 which are essential for normal hair growth
Anatomical Blurb: Hair Growth Cycle
- Anagen (85% hairs) : 2-6 yrs, hair growth beginning in the dermal papillae, pushing older cells out of the follicle
- Catagen (1-2% hairs): 1-2 wks, follicles shrink to 1/6th of normal length, lower part destroyed → dermal papilla breaks away, detaching from blood supply
- Telogen (10-15% hairs): 5-6 wks to 4 mos, dermal papillae in resting phase and hair follicles are dormant
- Exogen (5% hairs): 2-5 mos, existing hairs fall out and are shed, new hairs reenter anagen phase (normal rate of shedding: 100 hairs/day)
Pathophysiology:
- Androgenetic alopecia (“pattern hair loss”): diminishing of anagen-telogen ratio → hair follicle miniaturization, finer hair shafts as terminal hairs are replaced with vellus hairs
- Excessive DHT (dihydrotestosterone) is partly responsible for shortening anagen, particularly in male pattern hair loss
- Female pattern hair loss may be attributed to increased androgen receptor susceptibility
- Alopecia areata: immune-mediated mechanisms induce early release from anagen phase and abruptly into catagen/telogen
- Involvement of interferon-gamma and substance P as potential pro-inflammatory agents
- Telogen effluvium: shortened anagen with premature shift into telogen → diffuse shedding after 2-3 mos; usually self limiting
Major Subtypes: Nonscarring Alopecias
Androgenetic Alopecia (male or female pattern hair loss)
Most common form of alopecia; slow and progressive hair loss; will see changes in hair diameter (in contrast to other forms of alopecia)
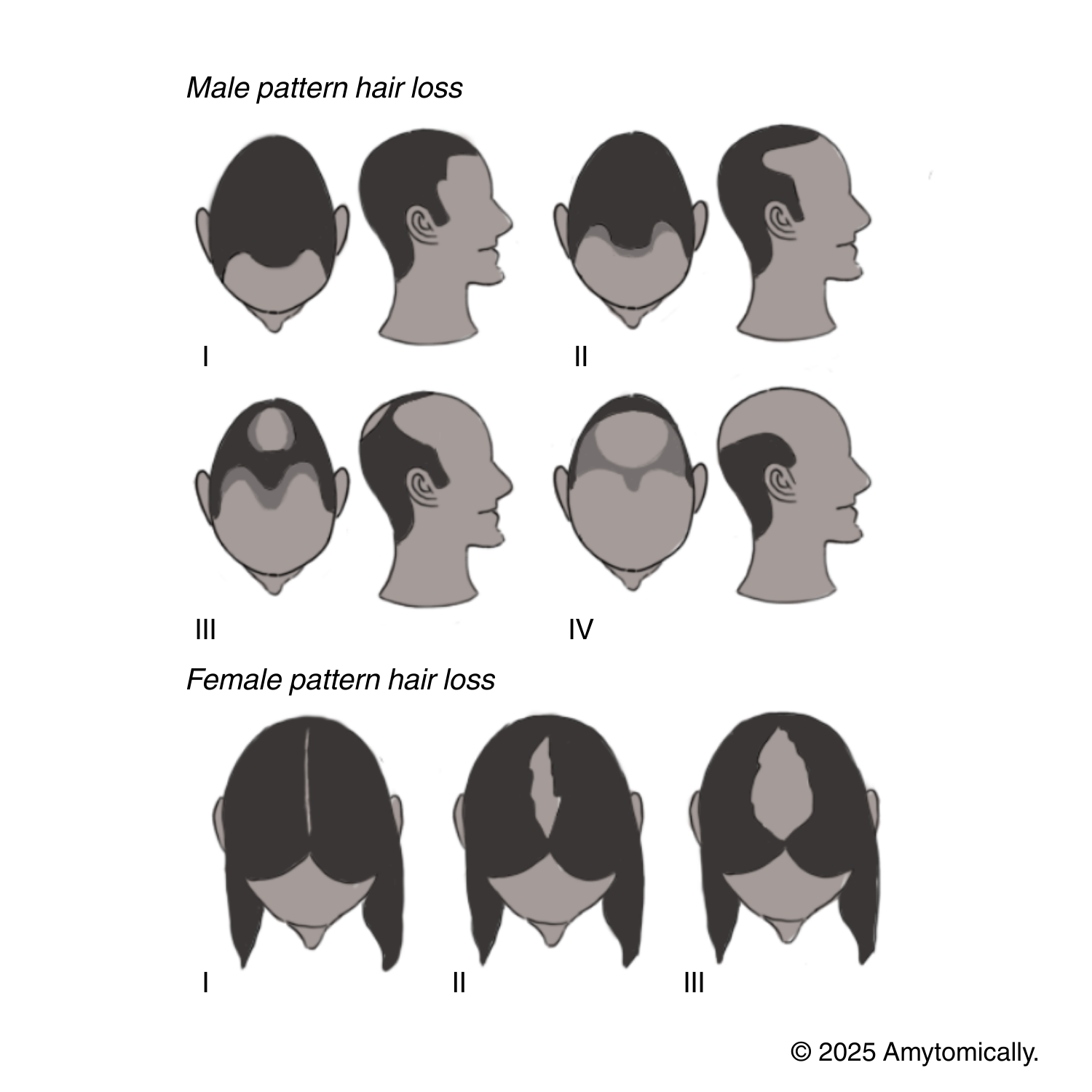
Male pattern hair loss (classified under Hamilton-Norwood Scale): hair loss affects midfrontal/bitemporal regions (see Image: II) and center (III), regions, resulting in characteristic M shaped hairline recession that meets with balding in the middle of the head (IV)
Female pattern hair loss (classified under Ludwig Scale): hair loss affects whole scalp in “Christmas tree” pattern down middle vertex (see Image: III), minimal involvement of just the hairline
Negative hair pull test
Alopecia Areata
Patchy hair loss at all ages, no pattern without inflammation
Totalis: complete scalp hair loss
Universalis: hair loss of entire body
Positive hair pull test (performed at patchy region)

Telogen Effluvium
Hair loss over entire scalp with inflammation
Entirely reversible when treating the trigger or underlying disorder after 3-6 mos shedding ceases if acute telogen effluvium
Positive hair pull test (indicates active shedding)

Treatment
Androgenetic Alopecia
Minoxidil/Rogaine (OTC): helps prevent progression of future hair loss but bad for regression that already occurred
Finasteride/Propecia: inhibits conversion of testosterone to dihydrotestosterone (DHT)
Spironolactone: blocks androgen receptors and weakly inhibits androgen synthesis
First line treatment for males (minoxidil, finasteride) vs females (minoxidil)
Others: platelet-rich plasma, hair transplantation, treating underlying nutritional deficiencies
Alopecia Areata
Treatments target and diminish abnormal immune reactivity
First line treatment: topical corticosteroids (e.g. triamcinolone acetonide)
Telogen Effluvium
Treat underlying disorders or removal of trigger
- Treat hormonal causes, such as hypo/hyperthyroidism
- Stopping birth control
- Diet regulation
- Regulate use of some medications such as NSAIDS or beta blockers


Leave a reply to amy’s biggest fan! Cancel reply