Burns
General Information
What is it?
Skin injuries primarily due to excessive heat, toxic chemical agents, electricity
Causes
- Thermal burns (~86%)
- Dry heat (open flame, explosion)
- Wet heat (scalding liquids, steam)
- Electrical (~4%)
- Chemical (~3%)
- Others: radiation, frost bite, aerosal inhalation
Evaluation
- Symptoms: see classification
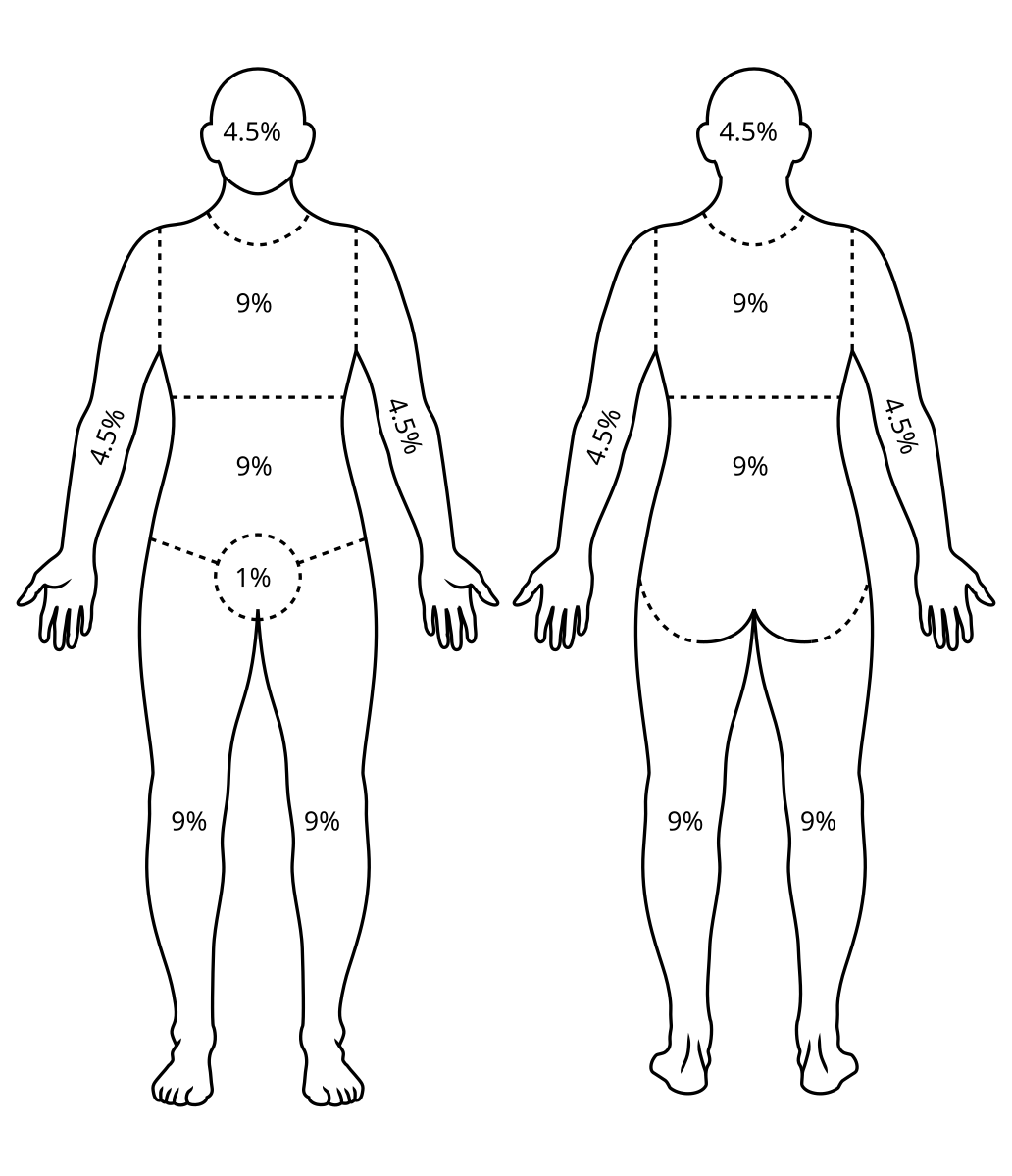
- Assessing total body surface area (TBSA)
- Rule of 9s: sum affected areas to determine extent of burn (refer to Lund & Browder Chart; i.e., Figure 1)
- Palmar method: palm represents 1% of body surface area, better for scattered burns
- Check airways for soot, particles
- CO, CN levels
Classification: see below
Pathophysiology: stages of zone penetration
- Coagulation: point of maximum damage; irreversible tissue loss or necrosis due to protein coagulation
- Stasis: diminished perfusion or ischemia; if not reversed (increasing perfusion) can progress to full necrosis
- Hyperemia: tissue perfusion increased, invariable recovery
Classification & Symptomatology

Burns can more generally be classified into the depth-based system of superficial burns and deep burns (which can range from partial to full thickness)
There is also a degree system (1st, 2nd, 3rd degree burns referencing superficial burns, deep/superficial partial burns, and full burns, respectively), but it is less common and precise
General categorization (superficial vs deep)
Superficial burns (Figure 1)
- Damaged keratinocytes recruits mast cells, macrophages which secrete pro-inflammatory cytokines
- Can stimulate nerve endings of nociceptors, causing pain
- Increases vascular permeability and decreased fluid retention
- Causing interstitial edema/hypotension, blistering on surface
- Cytokine-mediated vasodilation also causes erythema and blanching (after palpating skin, color returns to normal)
Deep burns
- Can affect and damage vasculature, producing dry non-blanching surface
- Little to no pain (hypesthesia) since nociceptors are likely damaged
- Also interstitial edema/hypotension due to increased vascular permeability
Specific categorization
Superficial: limited to epidermis
Dry, erythematous
Example: sunburns (peel by day 4, heal by day 6)
Superficial partial: epidermis, upper papillary dermis
Blisters, rupturing (fluid, weeping), erythematous
Extremely painful
Example: burns due to hot surfaces/liquids/flames
Deep partial: epidermis, upper papillary, and deeper reticular dermis
Easily rupturing blisters
Pale/white surface if lose vasculature
Likely no pain
Example: due to flames/superheated gas
Full: epidermis, dermis, and extends to hypodermis
Leathery, waxy, white/charred with eschar, no blanching
No pain
Treatment
General
Replace fluids/electrolytes
Treat respiratory distress after airway analysis
Cool via water/saline solution
When to refer to burn unit? If chemical/electrical/inhalation-induced burn, burn depth (full thickness, >10% TBSA), pregnant
By burn depth
- Superficial: OTC aloe vera, analgesics, NSAIDs for pain → little to no scarring
- Superficial partial: debridement, topical antimicrobials, non-adherent dressing, tetanus booster → minimal scarring
- Deep partial: fluid resuscitation, moist dressings, debridement, topical antimicrobials, grafting if necessary → higher risk of hypertrophic scarring
- Full: requires excision and graft → require surgical treatment
- Graft options:
- Split thickness graft: transfer of epidermis and superficial dermis
- Full thickness graft: transfer of entire epidermis/dermis; for small, cosmetically important regions (eyes, face, hands)
- Graft options:


Leave a comment