Myocardial Infarction
General Information
What is it?

Colloquially “heart attack”, characterized by complete or partial ischemia to a portion of the heart muscle/myocardium
Risk Factors: *underlying ischemia heart disease or coronary artery disease/CAD (most commonly, secondary to atherosclerosis), smoking, hypertension (HT), diabetes mellitus, lack of physical activity, alcohol abuse, hyperlipidemia, LV hypertrophy
Evaluation:
- Symptoms:
- Chest discomfort, angina (that may radiate into left arm, left jaw, or left neck), epigastric pain (if inferior STEMIs)
- Autonomic reflexes: nausea, vomiting, diaphoresis, syncope
- *EKG evaluation:
- ST segment elevation in two contiguous leads
- ST segment depression
- Biomarkers: *Elevated troponins
- Imaging (to examine myocardial thickness and perfusion): echocardiography (ECG), cardiac MRI
Classification: see below
Pathophysiology:
- Ischemic heart disease/coronary artery disease: occlusion in coronary vessels diminishes O2 supply and increases its consumption, leading to hypoxia (disrupting sarcolemma structure) → liquefactive necrosis
Classification
Categorization by region
Right ventricular MI (RV MI):
Leads to backflow into superior/inferior vena cava
Presentation: jugular venous distension, hepatomegaly, edema, hypotension (due to diminished SV, CO), sinus bradyarrhythmia/AV block (due to diminished conduction capacity at SA/AV node due to RCA occlusion)
Left ventricular MI (LV MI):
Blood backs into pulmonary vessels, causing edema
Presentation: dyspnea, decreased ejection fraction/EF (causes reflex tachycardia due to stimulation of ANS) s4 sound prominence, cold extremities, cyanosis
Categorization by EKG*
Non-ST-elevation MI (NSTEMI):
Myocardial necrosis without persistent ST elevation (troponin elevation): instead, may present with ST depression, T-wave inversion
The infarction is typically subendocardial (where necrosis due to ischemia begins)
Causative agent: typically thrombus formation which leads to ≥90% occlusion
Pain at rest
ST-elevation MI (STEMI):
Myocardial necrosis with persistent ST elevation, and potentially LBBB
The infarction is typically transmural (encompasses full thickness of myocardium, not just subendocardial)
Causative agent: thrombi/emboli that leads to total occlusion
*NSTEMI and STEMI also fall more broadly under categories of ischemic heart disease, as acute coronary syndrome.
Complications
Categorized based on 24h mark: when major complications tied to necrosis begin to appear, and coagulative necrosis is well underway
Within 24h
- Increased tissue permeability → increase frequency of APs → ventricular tachycardias (potentially VF)
- Other arrhythmias: reflexive tachycardia, SVTs,
- If LV MI: hypotension, cold extremities
- Cardiogenic shock
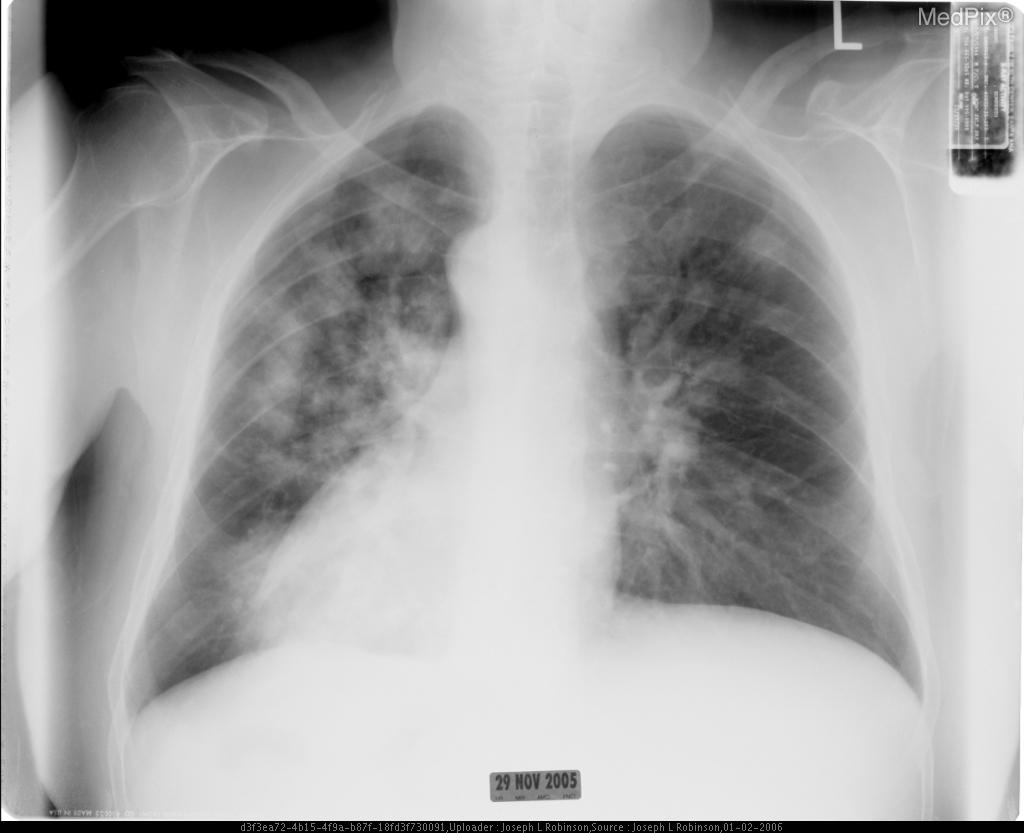
- Pulmonary edema (Figure 2)
- Reperfusion injury: free radical and calcium overload secondary to intervention
After 24h
- Interventricular septal rupturing → holosytolic murmur
- Free wall rupture → LV blood enters pericardial cavity → cardiac tamponade → triad (hypotension, jugular venous distension, muffled heart sounds)
- Papillary muscle rupture → severe mitral regurgitation/MR
- Pericarditis
- Arrhythmias
Treatment
Acute management
Reperfusion therapy
- Particularly essential for STEMI: Primary PCI (<120 min), fibrinolysis
- NSTEMI: fibrinolysis is contraindicated
Pain relief: intravenous opioids
Adjunctive medication: beta blockers, anti-coagulents, antiplatelets (especially aspirin), nitrates
Long term management & lifestyle modifications
Treat causative agent of CAD (likely atherosclerosis): statins to reduce LDLs, stabilize plaques
Medication: ACE inhibitors, beta blockers, glucose-lowering therapy if diabetic
Smoking cessation, weight control, minimize alcohol consumption


Leave a comment