Valvular Heart Diseases
General Information
*Note that Rheumatic Fever is not discussed here.
What is it?
Valvular heart diseases are pathological conditions that affect the heart’s valves. The most common valvular heart diseases are those affecting the aortic valve (aortic stenosis/AS and aortic regurgitation/AR), as well as those affecting the mitral/bicuspid valve (mitral stenosis/MS and mitral regurgitation/MR).
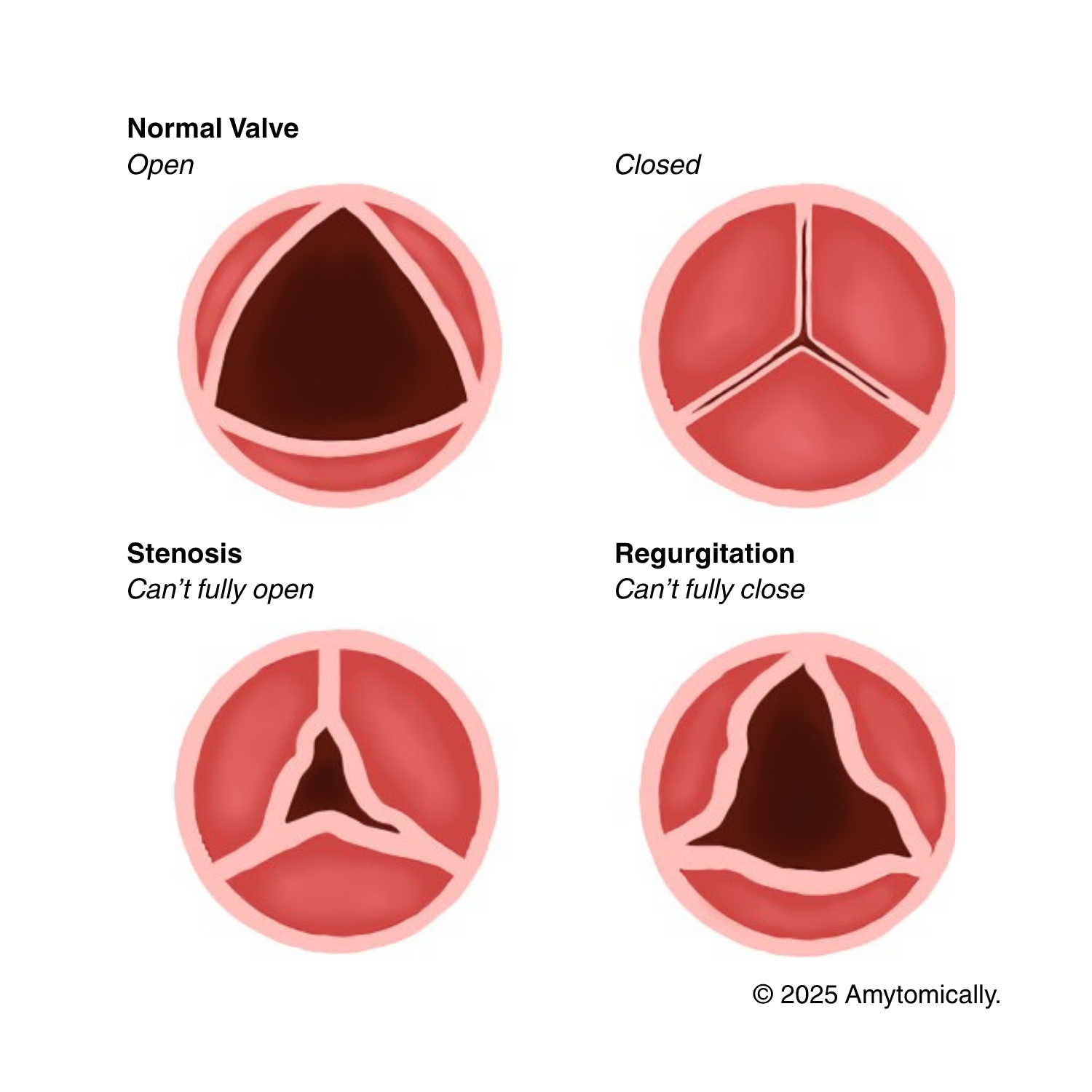
- Stenosis: sclerosis/fibrosis of tissue hardens and narrows the valve, preventing proper perfusion of blood between heart chambers
- Regurgitation: back flow of blood through valves that don’t properly close in between cardiac phases
Risk Factors: genetic (e.g. congenital valvular diseases such as bicuspid aortic valve), smoking, hypertension, older age (accumulation of calcium deposits)
Evaluation:
- Symptomatology differs based on the location and type of disease:
- AS: syncope and angina (due to lack of blood perfusion to brain and the coronaries, respectively), dyspnea (if blood backs up into the pulmonary circuit, causing pulmonary embolism)
- AR: dyspnea (also secondary to pulmonary embolism), cardiogenic shock
- MS: downstream effects of emboli (e.g., stroke, ischemia), PE, dyspnea, orthopnea (due to backflow into pulmonary circuit)
- MR: PE, overt cardiogenic shock
- Pulses & murmurs:
- AS: towards right sternal border at second intercostal space; weak carotid palpitations (pulsus pervus et tardus)
- Crescendo decrescendo, radiating to carotids
- AR: Decrescendo towards right sternal border at second intercostal space; water hammer/Corrigan pulse (extreme pulses during systole due to stretching of heart, and dropped pulse/completely flat during diastole as blood regurgitates)
- Can also present with the de Musset sign (subtle head bobbing), the Quincke sign (pulsations on fingernails), or the Muller sign (pulsations of the uvula)
- MS:
- Opening snap (after S2) with decrescendo rumble
- MR:
- Holosytolic murmur, radiating to axilla
- AS: towards right sternal border at second intercostal space; weak carotid palpitations (pulsus pervus et tardus)
- Imaging
- For AS and AR: 2D echocardiogram with Doppler study
- Measuring aortic jet velocity, mean aortic valve pressure gradient, and aortic valve area
- EKG
- For MS: abnormal P waves indicating LA enlargemet
- Chest x-ray
- For AS and AR: 2D echocardiogram with Doppler study
- Laboratory Pearls
- Increased B-type natriuretic peptide/BNP in MR
Etiology
Aortic Stenosis
If incidence <70yrs: likely due to valvular development (e.g., bicuspid aortic valve)
If incidence >70yrs: likely due to dystrophic calcification
- Calcification pathophysiology: damage and inflammation to the valve leads to the establishment of a collagen matrix
Can also be secondary to acute rheumatic fever: indicated by the presence of aschoff bodies and anitschkow cells
Leads to left ventricular outflow obstruction → diminished cardiac output/systemic perfusion → high afterload → ventricular hypertrophy → can lead to downstream diastolic heart failure
Aortic Regurgitation
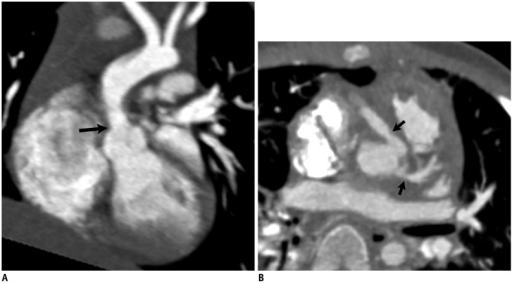
Caused by physical separation of aortic valve leaflets: due to dilation (e.g. ascending aortic aneurysm) or aortic inflammation (e.g. lupus)
Or by damage to valve: due to aortic dissection (if acute AR), infective endocarditis
Nosocomial causes: balloon angioplasties, transcatheter aortic valve replacements (TAVR)
Leads to excess preloard/afterload, generating wide pulse pressures

Mitral Stenosis
Primary cause: rheumatic fever
Since blood flow from LA to LV encounters high resistance with the stenotic valve → LA dilation → thrombi can be dislodged into emboli
Mitral Regurgitation
MR is divided into primary and secondary MR
- Primary (degenerative, organic): due to damage or structural pathologic changes to leaflets or leaflet apparatus (e.g. damage to papillary muscles, mitral valve prolapse/MVP)
- Secondary (functional, ischemic): due to LV abnormalities.dilation rather than the valve (e.g. systolic HF with reduced ejection fraction or dilated myopathies, which physically reduce overlap of leaflets)
Or caused by mitral valve damage: infection, genetic CT disorders (e.g. Marfans)
Treatment
Aortic valvular diseases
Little success with medical therapies
AS:
- Valve replacement especially for severe diseases (but depends on LV function)
- TAVR or SAVR
AR:
- Valve replacement recommended regardless of LV functioning
- Vasodilatory therapy
- SAVR
Mitral valvular diseases
MS:
- Medical therapy for reducing risk for developing recurring inflammation or rheumatic fever
- Benzathine penicillin prophylaxis to prevent rheumatic fever
- Anticoagulant therapy to prevent consequences of thromboemboli
- Surgical/invasive treatments: percutaneous mitral balloon valvuloplasty (PMBV), mitral valve replacement surgery
MR:
- Medical therapies have differing results
- Surgical treatments: mitral valve repair or replacement (with mechanical prostheses)
- Anticoagulants post-op


Leave a comment