Supraventricular Tachyarrhythmias
General Information
What are they?

They are tachyarrhythmias (above average heart rate and abnormal heart electrical activity) that originate above the AV node, atrial origin, or AV junction origin. To understand the heart’s conduction system and electrical pathways, please review this post.
Risk Factors: medications, stimulants (i.e. caffeine), stress, heart damage or trauma(increases likelihood of reentrant circuit formation and remodeling), congenital heart diseases
Evaluation:
- Symptoms:
- Tachycardia (180-220 BPM)
- *EKG evaluation: varies accordingly to arrhythmia (see below)
- All supraventricular tachyarrhythmias are characterized by a QRS complex of <120ms and a >100 BPM HR
- For closer analysis of the normal EKG, see here
Classification:
Regular RR Interval
- Sinus tachycardia
- Supraventricular tachycardias (SVTs):
- Focal atrial tachycardia (FAT)
- Paroxysmal SVTs:
- Atrioventricular nodal reentrant tachycardia (AVNRT)
- Atrioventricular reentrant tachycardia (AVRT) or Wolf parkinsons white syndrome (WPW)
- Atrial flutter
Irregular RR Interval
- Atrial fibrillation (AF)
- Multifocal atrial tachycardia (MAT)
- Atrial flutter or atrial tachycardia with variable AV block (not discussed below)
Pathophysiology
Focal origin
Characterized by the presence of an ectopic foci (an irritable area on nodal/myocardial tissue) that can induce a separate, ectopic pathway
Seen in FAT, MAT
- FAT: 1 ectopic foci
- MAT: >1 ectopic foci
Reentrant circuit origin
Characterized by the presence of an additional conduction bundle which causes a separate self-sustaining electrical circuit
Seen in AVRT/WPW, AVNRT, Atrial flutter
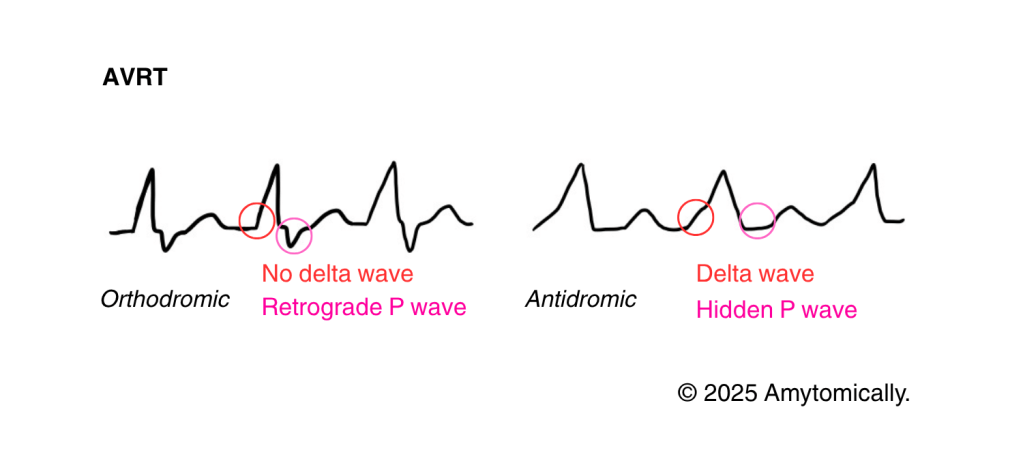
- AVRT/WPW:
- The circuit is typically present between the left atrium and ventricle, and is named the Bundle of Kent or James
- Orthodromic AVRT: after the AP reaches the purkinje fibers, it will into the accessory pathway and induce the arrhythmia; more common
- Antidromic AVRT: it goes opposite the typical AP pathway and is thus much more dangerous and fatal
- If alongside another fast tachycardic arrhythmia, the ventricular rate won’t be able to keep up with the atria
- AVNRT:
- Fibrosis and scarring can lead to the formation of two conduction paths down the AV node
- Alpha pathway (α): slow conduction (short refractory period)
- Beta pathway (β): fast conduction (long refractory period)
- The reentrant circuit is thus caused by reentrance into the alpha/slow pathway due to the beta/fast pathway’s long refractory period and then another switch, causing the signal to go back to the atria
- Slow fast AVNRT: from alpha to beta pathway
- Fibrosis and scarring can lead to the formation of two conduction paths down the AV node
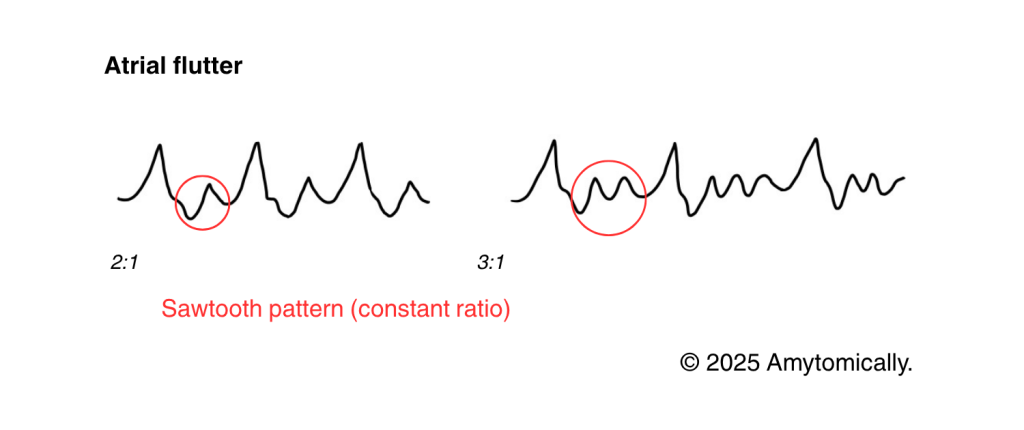
- Atrial flutter:
- Reentrant circuit present around tricuspid valve/annulus (cavotricuspid isthmus)
- The rate and ratio (i.e., 2:1 or 3:1) describes proportion of delay occurring at the AV node:
- 2:1 block (most common): 150 BPM
- 3:1 block: 100 BPM
- The rate and ratio (i.e., 2:1 or 3:1) describes proportion of delay occurring at the AV node:
- Reentrant circuit present around tricuspid valve/annulus (cavotricuspid isthmus)
EKG Analysis & Differential
Note that these are grouped by similar pathophysiology and etiology rather than by regularity (Figure 1) for ease of comparison.
Focal atrial tachycardia (FAT)
P waves inverted in VR or upright in AVR

Multifocal atrial tachycardia (MAT)

Atrioventricular reentrant tachycardia (AVRT)
Atrioventricular nodal reentrant tachycardia (AVRT)
P wave can come immediately after QRS (and is thus hidden), or it can form a Pseudo S or R wave if it comes close after. The Pseudo R wave (undepicted) is a result of the P wave superimposed on the terminal deflection of the QRS complex.

Atrial flutter
Regular atrial flutter presents with constant sawtooth (see below) in leads II, III, and avF. Irregular atrial flutter (undepicted) can have a variable sawtooth EKG pattern.
Sawtooth waves can present as positive (in V1), but are mostly negative (lead II).
Atrial fibrillation (AF)
See here.
Treatment
Vagal manuever (valsalva manuever): stimulates vagus nerve to slow down tachycardia
Pharmacotherapy: AV blockers (beta blockers, ca2+ channel blockers, adenosine) EXCEPT for WPW, AF, and atrial flutter patients
Anticoagulants for atrial flutter or AF
Last line: cardioversion to restore sinus rhythm (particularly recommended for AVNRT), ablation, chronic suppressive therapy


Leave a comment