Atrial Fibrillation
General Information
What is it?
It is a tachyarrythmia, and the most common arrhythmia. It primarily involves the heart’s upper chambers, the atria.
- “Tachy-” meaning above average heart rate (HR)
- “arrythmia” meaning abnormal heart electrical activity
Risk Factors: advanced age, underlying heart disease (e.g. myocardial hypertrophy or dilation, valvular diseases), ischemia, atrial inflammation, increased sympathetic atrial innervation, electrolytic abnormalities, hypertension (HT)
Evaluation:
- Symptoms:
- Irregular pulse, tachycardia (110-140 BPM)
- Examine airways and analyze cardiac biomarkers for differentials
- Blood test, CBC (for electrolyte abnormalities)
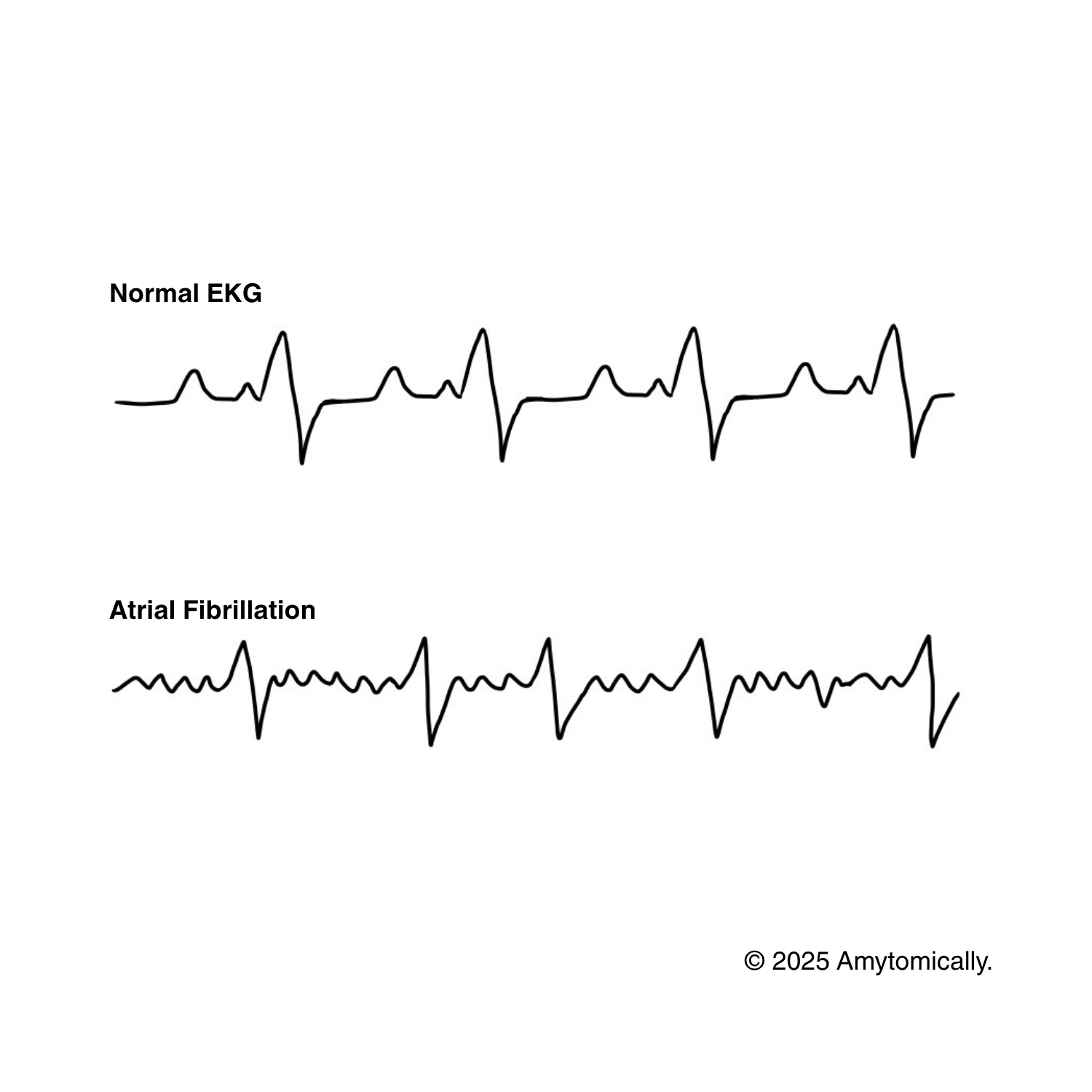
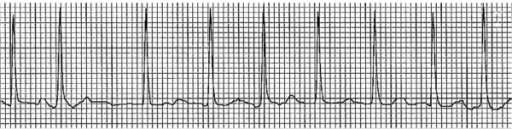
- *EKG evaluation: no distinguishable P waves and irregular R-R interval (see Figure 1)
- P wave irregularity indicates that depolarization is chaotic (due to reentrant circuits or ectopic foci)
- For closer analysis of the normal EKG, see here
Progression:
Paroxysmal AF: <7 days and self limiting (can return to sinus rhythm spontaneously, or via the elimination of the triggering foci)
Persistent AF: <7 days; requires heart remodeling (cardioversion)
Long standing & Permanent AF: >12 months; unresponsive to cardioversion (cannot revert to sinus due to permanently altered circuitry)
Causes & Etiology
PIRATE mnemonic for potential AF causes:
Pulmonary diseases, Infections, Remodeling of atria, Alcohol, Thyrotoxicosis, Electrolytic abnormalities
Cardiac causes
Defective heart structural remodeling (especially of the atria)
- Ischemic heart disease, congestive heart failure, or myocardial infarction (leads to stretching of myocardium): hypertrophy can lead to formation of reentrant circuits/ectopic foci
- Dilated myopathies (also increase stretch)
- Valvular diseases: atria hypertrophy due to retained blood (as decreased perfusion through stenotic valves)
- Hypertension (HT): atrial hypertrophy leads to remodeling
Noncardiac causes
Genetic causes–potential involvement of 10q22-q24: gain-of-function (GoF) mutation that increases pore concentration, increasing ion permeability and thus electrical instability
Hypoxia–ischemia/hypoxemia can induce cells around the left atrium to develop ectopic foci
Increased sympathetic (SNS) innervation–drugs such as catecholamines, methamphetamines can increase sympathetic activity or directly stimulate atrial cells (via B1-adrenergic receptors) and cause agitation
Electrolytic disturbances–low K+ or Mg2+ can trigger ectopy
Alcohol consumption (Holiday Heart Syndrome)–high alcohol concentration leads to increased reactive O2 species, leading to atrial inflammation, increased sympathetic activity, and electrolyte alterations
Complications
Thromboembolic
- Thrombus formation due to static blood flow in atria → can lead to *stroke (if lodges in brain), mesenteric ischemia (if in mesenteric arteries), acute limb injuries (if in extremities)
- For estimating stroke risk, the CHADs-2-Vasc score is employed:
- 0: low risk, anticoagulation not recommended
Heart failure
- Little filling time due to abnormally fast ventricular rate → diminished EDV, SV, CO → shock, low BP
- Can also lead to regurgitation back into atria and into the pulmonary system → dyspnea, orthopnea, hypoxemia
Treatment
For estimating stroke risk (and appropriate treatment for AF), the CHADs-2-Vasc score is employed:
- 0: low risk; anticoagulation not recommended
- 1: moderate risk; consider anticoagulants or antiplatelets
- 2: moderate-high risk: recommend anticoagulation therapy; anti-arrhythmias
Rate control medication (block AV node): beta blockers, Ca2+ channel blockers, digoxin, amiodarone
Rhythm control medication (only if hemodynamically unstable): cardioversion (amiodarone, flecainide), radial ablation (to remove damage of remodeled pathways)
Anticoagulation: DOAC (nonvalvular etiology), warfarin (valvular)
Pacemaker (only if very severe, and if CHF implicated)


Leave a comment