Abdominal Aortic Aneurysm (AAA)
General Information
What is it?
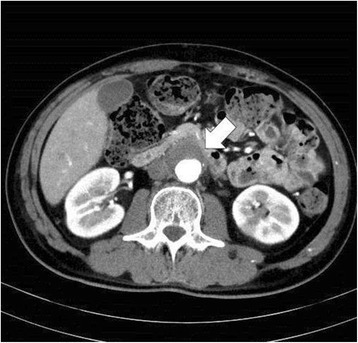
High morbidity enlargement and dilation of a region of the abdominal aorta (150% of normal diameter), with risk of rupture proportional to size
Risk Factors: atherosclerosis*, white male, smoking, older age (>60), high BP/cholesterol/obesity, history of aortic dissection (AD)
Small AAAs are classified as 3-5cm, with the rate of rupture increasing significantly for every size increase
Saccular (localized) vs Fusiform (circumferential)
Evaluation:
- Enlargement rate
- 0.2/0.3cm per year
- Symptoms
- Majority of afflicted individuals are asymptomatic
- Shock, abdominal pain, distension
- If ruptured: gastrointestinal (GI) bleeding, CHF
Pathophysiology & Etiology
- Primarily due to weakness in structural integrity of aorta (e.g., elastin, collagen)
- Thus, the infrarenal region may be more likely to be compromised because it has a lower number of collagenous lamellar units
Anatomical Blurb: Aorta Anatomy
The aorta, the strongest and largest artery in the body, is divided into subcomponents from its origination at the left ventricle (and the aortic valve).
- The aortic arch: the ascending and descending aorta (subclavian, carotids, and brachiocephalic trunk originate here)
- The thoracic aorta: chest cavity (wall, esophagus, bronchi)
- The abdominal aorta: supplies abdominal organs (stomach, intestines, kidneys, liver, etc)
Treatment
Surgical approach
Recommended for non-ruptured aneurysms <5-5.5cm, or when they become symptomatic
Endovascular repair/EVAR (using femoral artery), open repair (graft affected aortic region)
Non-surgical approach
For small aneurysms, can introduce lifestyle modifications: control BP and cholesterol, exercise, diet
Physiological Blurb: Aneurysms
Aneurysms are expanded and bulging blood vessels, that may have high risk of rupturing.
Complications: blood stasis promotes thrombi or emboli formation, life-threatening hemorrhage, related organ/tissue damage
Potential complications: ischemia, MI, amputation, death, impotence, surgical complications (vascular injury or nicking, breakdown of graft material), renal insufficiency


Leave a comment