Peripheral Arterial Disease (PAD)
General Information
What is it?
Diminished perfusion and ischemia of peripheral arteries (and thus the body’s extremities)
Risk Factors: atherosclerosis*, diabetes, smoking, older age, high BP/cholesterol/obesity
Evaluation:
- Symptoms:
- Pain and cramping of lower extremities due to persisting ischemia/occluded perfusion
- Ischemic rest pain due to poor perfusion to nerves (burning pain in the feet)
- Ulcers, gangrene
- Muscle atrophy
- May be asymptomatic
- Physical exam
- Diminished/absent lower extremity pulses
- *Ankle Brachial Index: much smaller ABI (<0.9)
- Diminished/absent lower extremity pulses
Primary Causes
*Atherosclerosis
Plaque formation (for pathophysiology, see Atherosclerosis) most commonly in abdominal aorta, iliac, femoropopliteal, and tibiofibular arteries
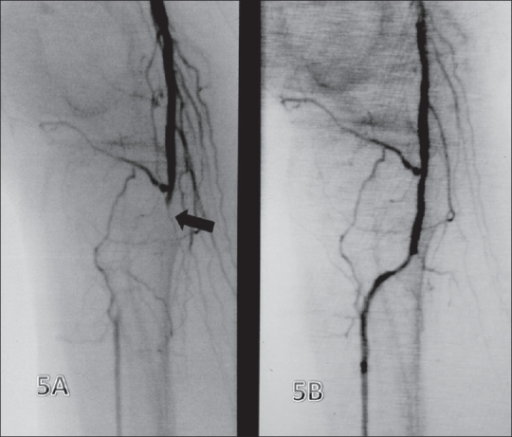
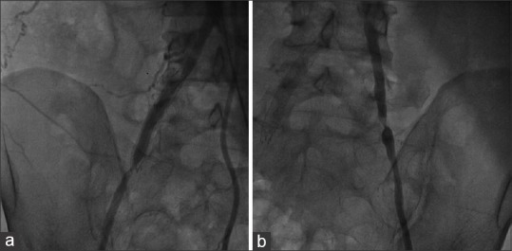
Pathophysiology of PAD: (1) Atherosclerotic blood vessel occludes blood flow (2) Arteries compensate by dilating until even dilation cannot compensate for lumen narrowing (3) Thrombi/emboli may form on the plaque wall (3) Tissue infarction resulting from unresolved ischemia
Emboli (secondary to atherosclerosis or similar causes)
Most commonly found in femoral and iliac arteries, as well as the aorta and popliteal arteries
Common complications: AAA, popliteal aneurysm, compartment syndrome, lower extremity pain
Complications
S1. Claudication
- Plaque only partially covers vessel
- Pain on exertion and is limited to area surrounding affected vessels with thrombi (e.g. compromised femoropopliteal artery leads to corresponding calf pain)
S2. Critical Limb Ischemia
- Plaque occludes majority of lumen, significantly limiting blood perfusion
- Pain at rest and is chronic; is present in other areas (i.e. hair, skin → hair loss, skin necrosis/ulcers)
S3. Acute Limb Ischemia
- Plaque has dislodged, forming thrombi and/or emboli
- Immediate/acute ischemia
- Pain at rest
- Recognizable by 5 Ps: pain paralysis, parasthesias, pulseless, pallor
Treatment
Lifestyle changes to reduce risk of further cardiovascular disease (CVD) complications such as MI, stroke, thrombosis: reduce, diet modification to regulate cholesterol and hypertension
1. Exercise therapy
2. Medications: cilostazo (promotes vasodilation), heparin (prevent clot from enlarging)
3. Treat atherosclerosis: statins, endovascular and revascularization treatments (angioplasty/stenting, bypass grafts to divert flow around blockage)
4. If nonviable limb: amputation


Leave a comment